The Skeleton of Harry Eastlack
The skeleton of Harry Eastlack (1933 – 1973), a man who
lived with FOP until he died just six days short of his fortieth birthday, is
on display at The Mutter Museum of The College of Physicians in Philadelphia.
At age 5, he broke his left leg while playing with his sister.
There were complications with the fracture, which did not set properly. The hip
and knee stiffened and bone growths began to develop on the muscles of his
thigh. Within some years the condition spread to other parts of his body, ossifying
his tendons and muscle and fusing his joints. By his mid-20s his vertebrae had
fused together. He died from pneumonia in November 1973, six days
before his 40th birthday. At the time of his death his body had completely
ossified; even his jaw locked up, leaving him able to move only his lips.
Late in his life, Harry Eastlack made the decision to bequeath
his body to his physician who donated Harry's skeleton to The Mutter Museum so
that physicians and scientists in future generations could study and learn
about FOP. Unfortunately, when Harry was alive, he never met another person with FOP. Harry
Eastlack's skeleton, one of the few existing in the world, has become a
valuable asset to physicians and scientists studying Fibrodysplasia Ossificans Progressiva (FOP).
The glass case in which Harry Eastlack's skeleton dwells has
become a window into the medical mysteries and scientific challenges of FOP. It
also exemplifies the harsh reality of FOP more than any chart, slide, or
clinical description could accomplish.
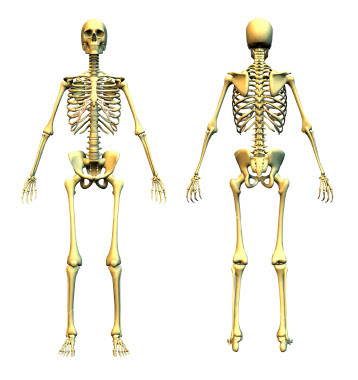
Normal skeletons collapse into piles of loose bones when the
connective tissues that join bones together in life are removed. To be
displayed in human form, skeletons have to be re-articulated or pieced back
together with fine wires and glue. As a result of the bridges of bone that
formed from FOP flare-ups, Harry Eastlack's skeleton is almost completely fused
into one piece, which proved little challenge for the articulator's craft.
Sheets of bone cover Harry Eastlack's back. Ribbons, sheets, and
plates of bone lock his spine to his skull and his skull to his jaw. Additional
ribbons and cordons of bone span from the spine to the limbs and immobilize the
shoulders, elbows, hips, and knees. Thin stalagmites of bone launch themselves
from his pelvis and thighs. His upper arms are welded to his breastbone by
slender white bridges of bone that cross his immobilized rib cage.
This FOP skeleton, which stands as Harry Eastlack stood in life,
is a constant reminder of how far scientists have come in the research of FOP,
but it is also a constant reminder of how much further they need to go.
Although no member of the FOP research team at The University of
Pennsylvania in Philadelphia ever knew Harry Eastlack during his lifetime, they
have come to know Harry well posthumously through his remarkable bequest. Dr.
Frederick Kaplan said that “Harry's skeleton is like The Sphinx. It stands
silently and elegantly and reveals its secrets if you ask the right questions,”….“When
we discover something important about FOP in the laboratory, we return to visit
Harry's skeleton in order to confirm the reality of the discovery. At other
times, we may discover something about Harry's skeleton that sends us running
back to the laboratory to test a new hypothesis about FOP,” Kaplan added. “The
gift that Harry has given to the FOP community is inestimable and his bequest
has given additional meaning and depth to medical and scientific research well
beyond the confines of his mortal existence. I never knew Harry in life,” added
Kaplan, “But I bless his memory every time I visit the museum where his legacy
continues to educate and inspire.”
Source: ifopa