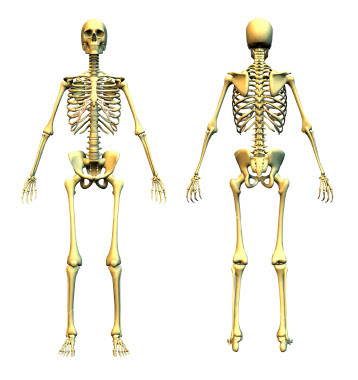
Before moving to the FOP related facts
and figures let’s try to understand FOP bones versus Normal bone.
FOP Bone versus Normal Bone
Bone is a living tissue. Each bone in our body is like an organ,
made up of tissues and cartilage. FOP bone is just like normal bone — but in
the wrong place.
Ossification (osteogenesis) is
the process of new bone formation. There are two methods of bone formation:
ü Intramembranous
ü Endochondral
Intramembranous bone formation is the simpler process, and it's responsible for
forming a person's skull and lower jawbone. It's also determine how long bones
like the ‘humerus’ and ‘femur’ grow in width.
Most bones in the body grow and heal after a break through
endochondral bone formation. It's
also controls how FOP bone grows. First, cartilage forms and then bone
gradually takes the place of the cartilage.
Both kinds of ossification begin with mesenchyme.
Mesenchyme is a connective tissue from which all other connective tissues come
from. Mesenchymal cells can turn into different kinds of specialized cells which
form tissues. The process of endochondral bone formation is as follows:
1.
Mesenchymal cells come
together in the shape of the bone they will form. They turn into chondroblasts —
cells that secrete cartilage matrix. A membrane called the perichondrium surrounds
this cartilage.
2.
After the chondroblasts
cover themselves in cartilage matrix, they turn into chondrocytes.
The chondrocytes keep dividing while new chondroblasts continue to make
cartilage matrix, causing the cartilage to grow.
3.
Some of the
chondrocytes burst and others die. The bursting of the cells causes calcification
or hardening of the cartilage. The dying cells make small spaces in the
cartilage.
4.
A nutrient
artery enters the cartilage, triggering cells in the perichondrium to
turn into osteoblasts. Osteoblasts are just like chondroblasts, but
they secrete bone matrix instead of cartilage matrix. The osteoblasts start to
secrete compact bone, and the perichondrium becomes the periosteum —
the cover of the outside of the bone.
5.
Blood vessels grow
into the cartilage and bring red bone marrow cells and other bone cells with
them. The blood vessels stimulate a primary ossification center to
grow — this is the place where bone tissue will begin to take the place of
cartilage. Osteoblasts start covering the broken-down cartilage with bone
matrix.
6.
Osteoclasts follow
behind the osteoblasts and break down the spongy bone, making a cavity for red
bone marrow to fill.
So, at this point, the long part of the bone, which started as
cartilage, is compact bone with red bone marrow in the center. The endochondral
bone formation finishes with the epiphyses, the ends of the bones.
Secondary ossification centers develop
to form bone, although unlike with the primary ossification center, spongy bone
stays at the center of epiphyses instead of marrow.
This process uses undifferentiated cells or cells
that can grow into any type of cell to make bones. The amazing thing about FOP
is that the body convinces undifferentiated cells in tendons, ligaments and
muscles to turn into something completely different. The body doesn't normally
work this way. With FOP, ligaments and tendons and other connective tissues all
go through this process of bone formation. It is normal bone, but in the wrong
place at the wrong time — this is called heterotopic ossification.
So
what happens with FOP?
A mutation in the gene encoding Activin receptor IA (ACVR1) tells the body to make an extra
skeleton. This gene is responsible I controlling helps ‘bone morphogenetic
proteins’ — BMPs. In FOP, the gene is active without BMPs —
operating like a leaky faucet. When BMPs are present, the faucet explodes with
activity. This clue might someday help scientists figure out how to make extra
bone for people who need it, like people with osteoporosis.